Para Hisian atrial tachycardia ablated from the non-coronary aortic sinus
David Gonzalez Casal , Adolfo Fontela , Nina Soto, Jorge González Panizo, Tomás Datino. Hospital Universitario Quirón-Salud & Complejo Hospitalario Ruber Juan Bravo, Madrid. Spain.
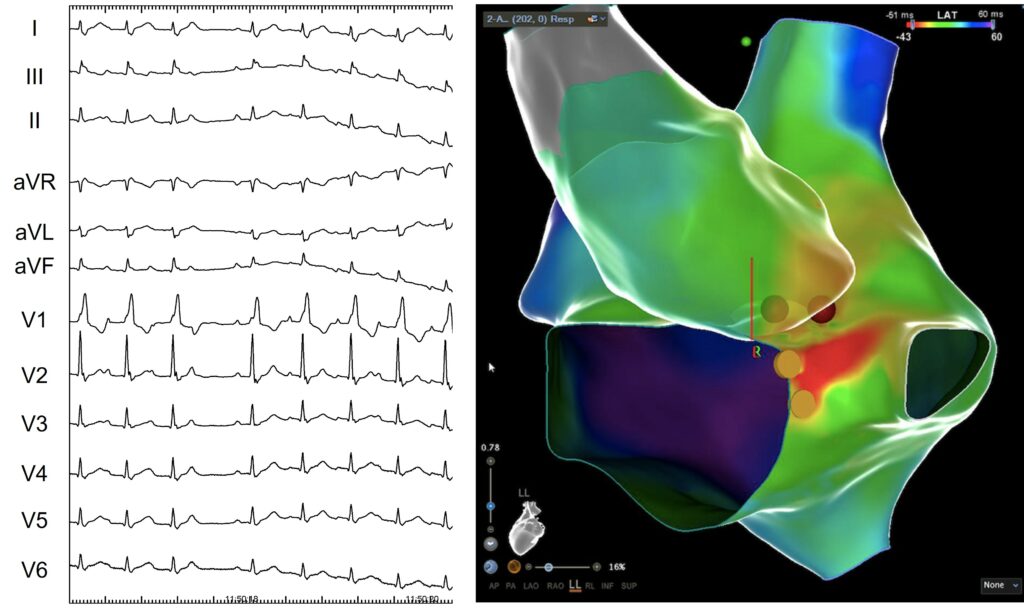
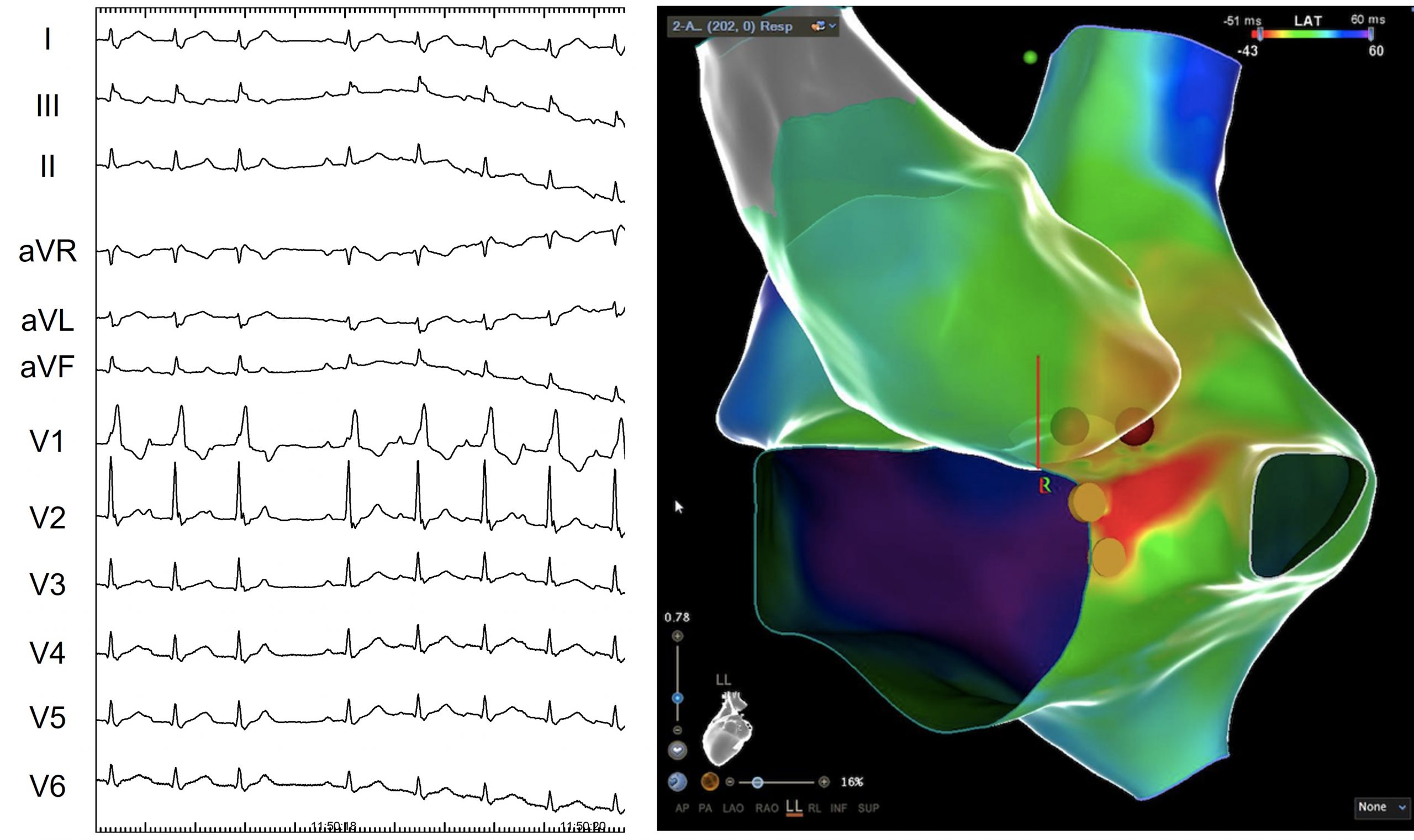
A 80 year old woman, without prior cardiovascular risk factors, and under treatment with levotiroxin after surgical removal of the thyroid gland as the only relevant medical history, was admitted to the emergency department of our hospital with symptoms of palpitations and dyspnea. While monitoring, multiple events of tachycardia were observed. A 12-lead EKG was performed during one episode showing a regular wide QRS tachycardia (right bundle branch block already present during sinus rhythm) and a long RP interval compatible with atrial tachycardia. The morphology of the P wave was thinner than those observed during sinus rhythm and biphasic in inferior leads and V1 (the negative component more prominent in inferior leads and the positive in V1).
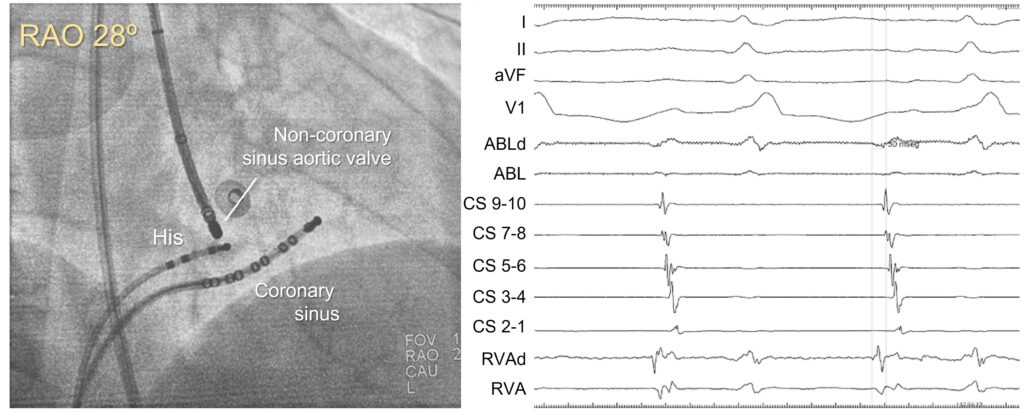
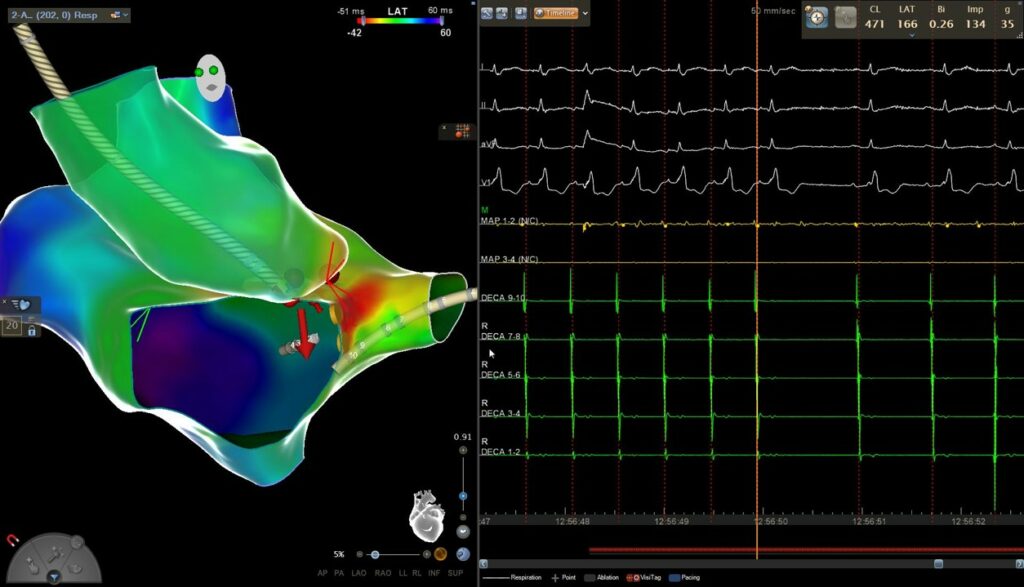
Atrial programmed stimulation was performed, after rapid burst pacing from the coronary sinus and the patient’s clinical tachycardia was induced in a reproducible fashion. Entrainment maneuvers were performed from the right ventricle apex with a consistent VAAV response after pacing, a finding compatible with the diagnosis of atrial tachycardia.
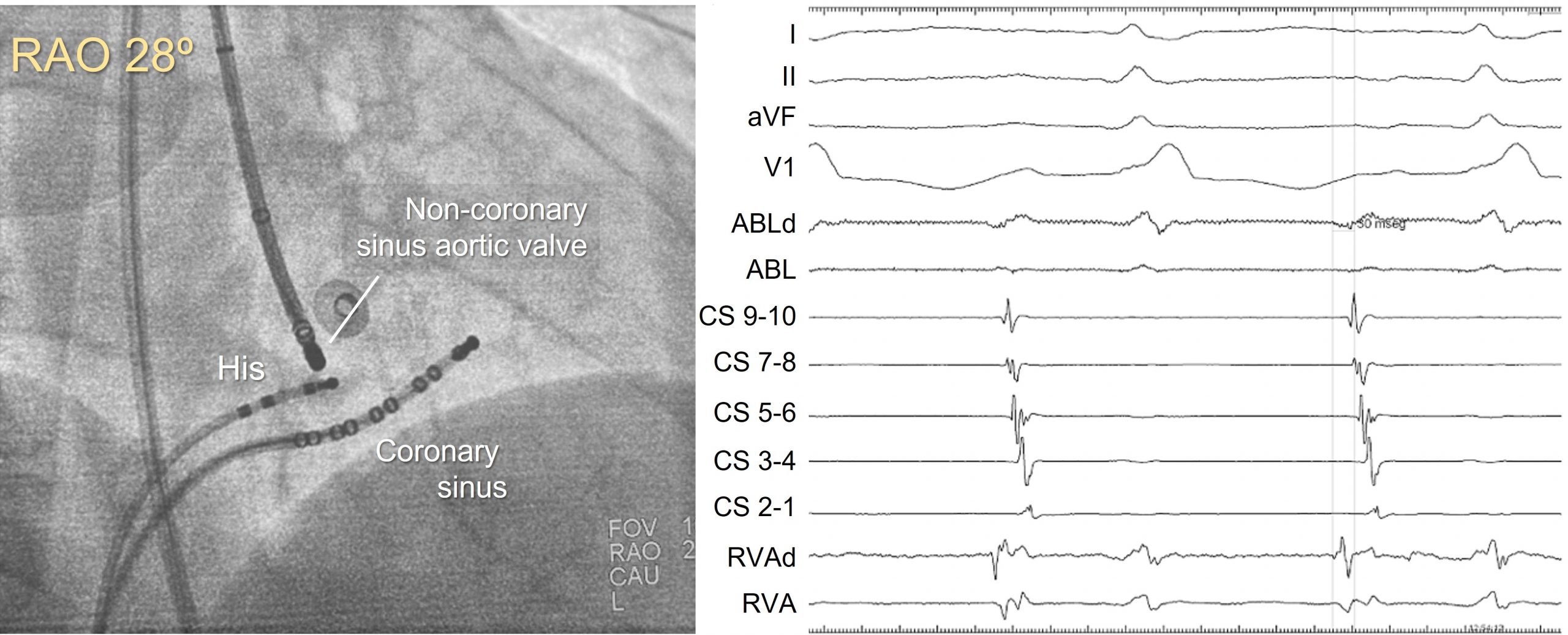
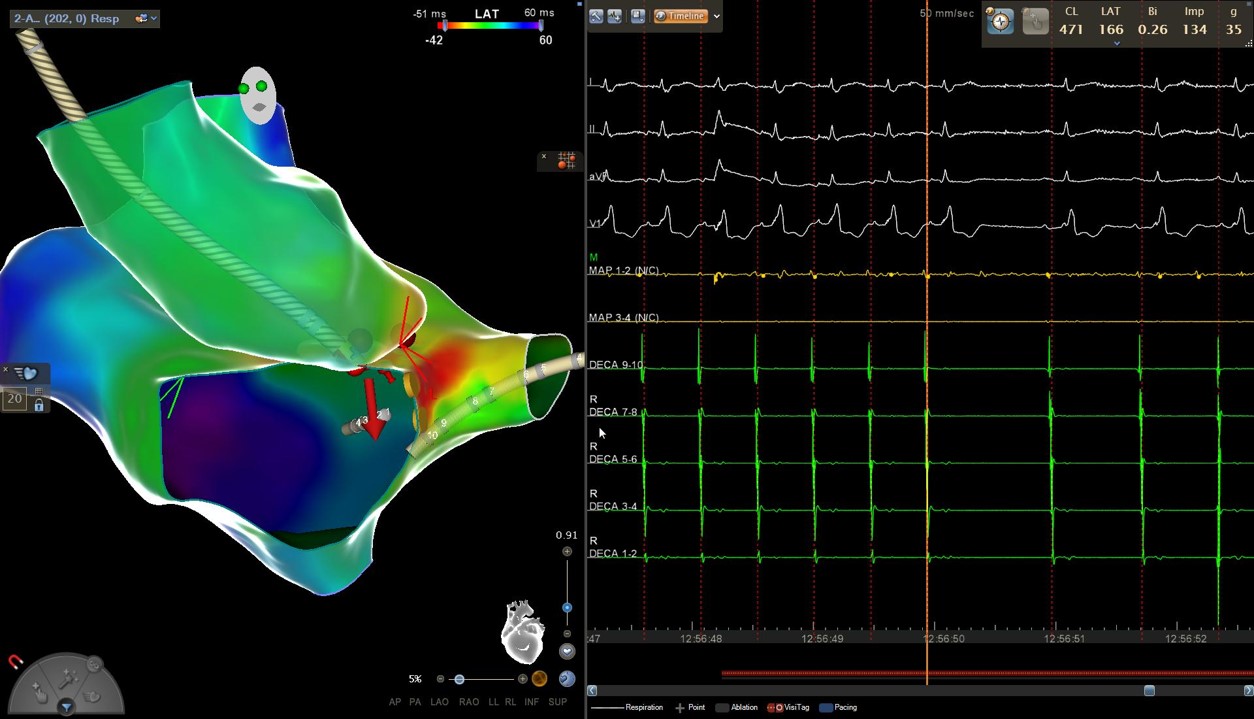
An electroanatomic reconstruction of the right atrium was obtained with the CARTO3 system, activation mapping showed that the region of greatest precocity was located at the vertex of the triangle of Koch, at the anatomical location of the penetrating AV bundle. At this point a His bundle potential was clearly recorded by the ablation catheter.
A new activation map of the aortic root was obtained. The greatest precocity was recorded in the non-coronary aortic sinus, where local atrium depolarization preceded the onset of the P wave by 30 ms, similar to those recorded in paraHisian areas of the right atrium. Initially, radiofrequency was carefully applied with an irrigated-tip catheter reaching up to 20W. Atrial tachycardia ceases during the application and sinus rhythm was maintained once it was finished.
Anatomical correlates
By Cabrera & Sánchez-Quintana
-
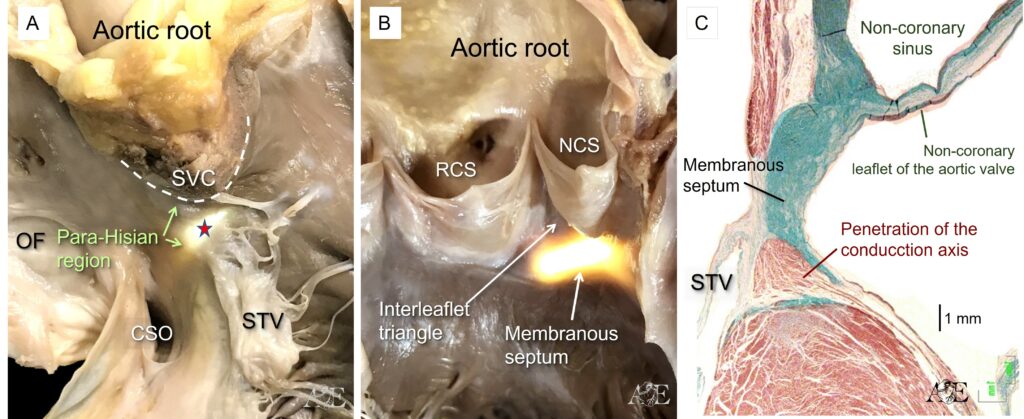
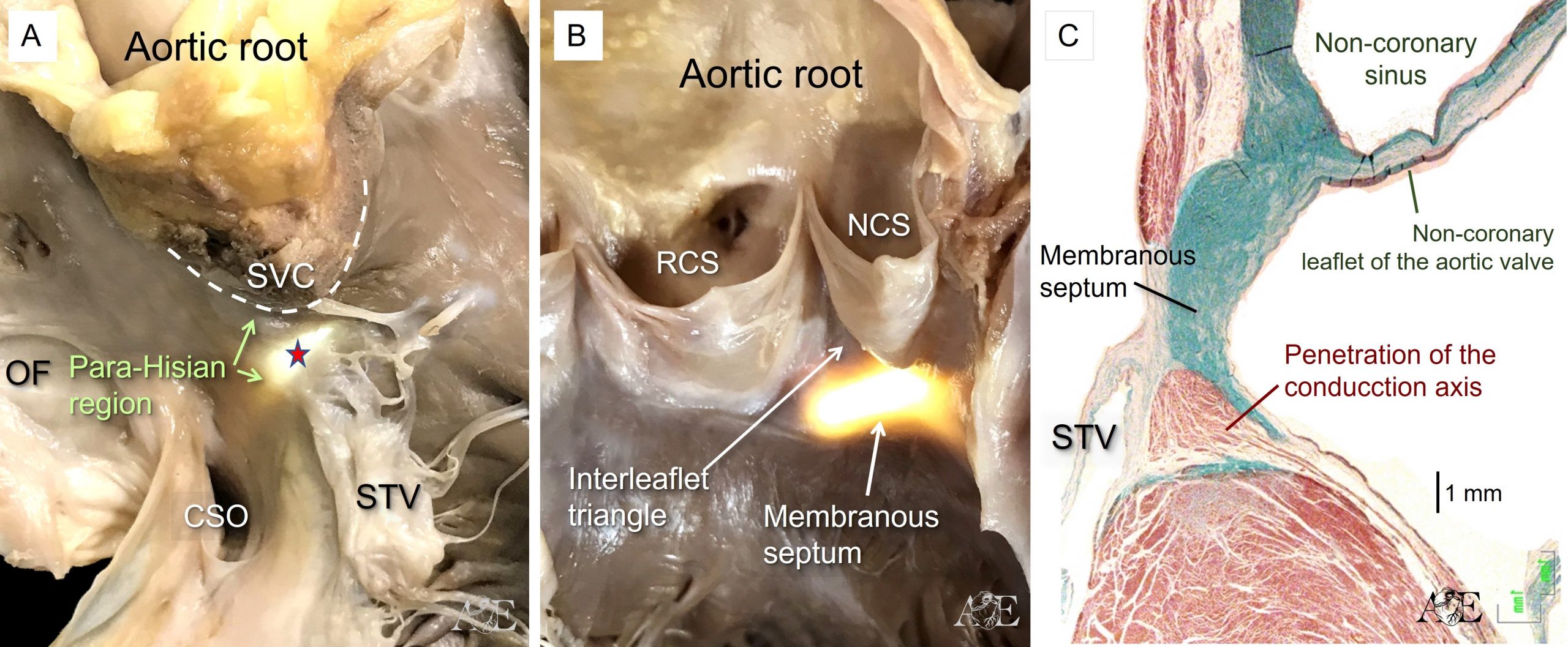
The areas surrounding the location of the penetrating Atrioventricular (AV) bundle constitute the para-Hisian region. This regions are directly adjacent to the transition of the AV conduction from the AV node from the non-branching atrioventricular bundle (Figure 4A-C). The figure 4A shows how the attachment of the septal leaflet of the tricuspid valve (STV) separates the septum (red arrow) into its atrioventricular and interventricular components. Note the anatomic relations with the supraventricular crest (SVC) the oval fossa (OF) and the orifice of the coronary sinus (CSO) in simulated right anterior oblique projection.
-
The superior para-Hisian area is directly related anteriorly to the non-coronary aortic sinus (NCS) and right coronary aortic sinus (RCS)
-
Sections taken cranially, cutting through the non-coronary aortic sinus, show the relationship between the hinge of the non-coronary leaflet of the aortic valve and the basal extent of the left bundle branch (Figure 4c). This histological section also shows the fibrous membranous septum that is the truly atrioventricular septal structure.